By Don C. Reed
As a kid, I spent a lot of time in hospital. Nurses were a big part of my life. Most were kind. But one was not a friend to children who asked too many questions…
I remember the day when a newcomer on a wheeled bed was shoved in next to mine: a pale little boy with his eyes shut.
But what interested me was the glass jar of red liquid suspended above him, and the plastic tube going down into his arm.
I was afraid of the nurse. But I was eaten up with curiosity.
“What is that?” I finally asked, pointing to the red jar.
The nurse looked over at the pale kid, then back to me. And she smiled…
“He gave trouble”, she said, “So we’re taking his blood out. You’re not going to give trouble, are you?”
In a couple days the pale boy went away. I never knew what happened to him. But I had nightmares about that nurse, and her vampiric blood jar…
You know, of course, what I did not understand: the child was just having a transfusion. They were putting blood in, not taking it out. (This was 1951, and some hospitals still used glass jars instead of blood bags.)
But what if there was no way of storing blood to use for such transfusions?
Numerous countries worked years on the problem. At the Battle of Leningrad in World War I, the Russians systematically stored blood for wounded soldiers. One Russian surgeon, Sergei Yudin, worked 20 years on the study of taking blood from cadaver. Unfortunately, he was jailed for political reasons, and his last two books were written in prison — on toilet paper!
The Russian work was studied by an American doctor, Bernard Fantus. In the early 1930’s Dr. Fantus worked at the Cook County Hospital in Chicago, Illinois. He married a nurse named Emily Senn, and they adopted a little girl, Ruth.
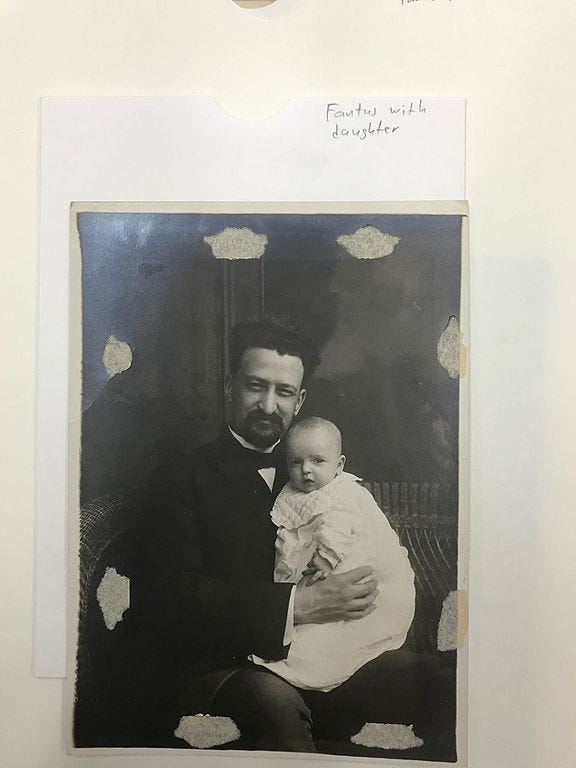
Bernard Fantus and His Daughter: picture courtesy “My Hero Bernard Fantus”
https://en.wikipedia.org/wiki/Bernard_Fantus#The_Blood_Bank[6]
Fantus began thinking about the need for blood, portable and storable, for all those soldiers, wounded in battle. He brooded about the possibilities.
He talked about it with his daughter, and one day little Ruth said:
“Why not call it a blood bank?”
In 1937, Dr. Fantus developed the world’s first blood bank. In World War II Two battles, many lives were saved, because of his stored and transfused blood.
But to this day, problems still remain.
What if there was no match between donor and recipient? Or if the blood was tainted by disease? Testing could detect much unsafe blood, but maybe not all.
What if, instead of borrowing blood from others, it was made from stem cells?
Dr. Tannishtha Reya of UC San Diego wanted to take on that challenge — if the funding could be found.
One of the most interesting grants given by the California stem cell program is the “Inception” award. This award “provides seed funding for great ideas that have the potential to impact human stem cell research, but need some initial support. It is hoped this will enable the researchers to test their ideas, and give them the data they need to compete for more substantial funding.” — CIRM Stem Cell Agency.

Dr. Tannishtha Reya: picture courtesy of stemcellpodcast.com
Dr. Reya was given an “Inception” Award, and she focused on developing Onegative type, red blood cells, which can be used by the vast majority of patients. A universally acceptable donor blood source would meet a serious need.
Because?
“Every two seconds someone in the U.S. needs a blood transfusion. But sometimes, due to a shortage of donors, there is not enough blood… and surgeries…have to be canceled.”
“Creating a safe, unlimited supply of universal donor blood cells could have a huge impact, not just in the U.S., but worldwide,” said Jonathan Thomas, Ph.D, J.D., Chair of the CIRM board of directors.
So how does Dr. Reya hope to meet this need?
Below is my layman’s understanding: from reading her papers, and a halfhour talk on the phone: how she can (hopefully!) make a universal blood supply.
First, bone marrow is where the blood is made, so she will need to take some from a healthy person, just one– and that person’s contribution may be all we ever need.
Then Dr. Reya will apply one specific gene to take the cells halfway to becoming blood. They are now a stem cellderived line of erythroblasts, the Eline.
They must stay as they are, and not change (differentiate) into red blood cells (RBCs) — not yet.
Here’s why. Erythroblasts can be multiplied cleanly; RBCs cannot.
She will multiply the “Eline”, making lots. Then, differentiate it — into clean, un-rejectable red blood cells. It is ready to use; transfuse where needed.
Of course, it is easier for me to say than for Dr. Reya to do! But the idea seems sound, and we wish her all success — if she wins, everybody wins.
P.S. One more story about the aforementioned Dr. Fantus. He hated to see children suffering needlessly, forced to swallow hatefultasting medicine. He kept thinking — why should medicine have to taste so vile and loathsome?
So, he contacted confectioners, professional candymakers and they came up with flavors and coatings more acceptable to kids!
Medical research: organized kindness: to save lives and ease suffering…
But it all takes money, which is why California’s Proposition 14 is so absolutely vital. Prop 14 will provide $5.5 billion to renew funding for the California stem cell program. That may sound like a lot, but it’s not — last year, according to no less than the CDC (Center for Disease Control and prevention) chronic disease cost America roughly $3 TRILLION dollars — 90% of all health care expenditures.
https://www.cdc.gov/chronicdisease/about/costs/index.htm
Remember in November: on election day, November 3, vote YES! on Proposition 14: the California Stem Cell Research, Treatments, and Cures Initiative of 2020.
Don C. Reed is the author of “REVOLUTIONARY THERAPIES” from World Scientific Publishing, Inc., 2020, and other stem cell books.